What Is Diverticulitis, And What Are The Symptoms
Diverticulitis is a common yet often misunderstood condition affecting the digestive system, marked by inflammation or infection of small pouches that can form in the walls of the colon, known as diverticula. This condition is significant, as it not only disrupts digestive health but also impacts overall wellness, leading to severe abdominal pain, changes in bowel habits, and even complications requiring surgical intervention. This article aims to shed light on this condition and equip readers with essential knowledge for better digestive health, encouraging proactive steps toward prevention and early diagnosis.
How Diverticulitis Develops and Why It Can Be Serious
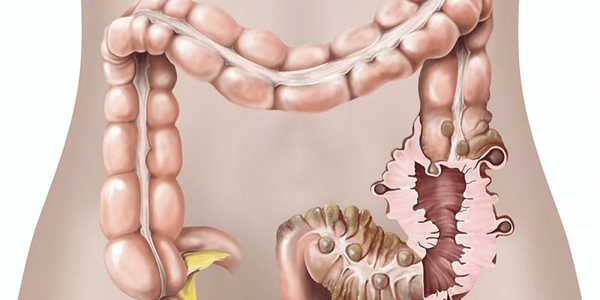
Diverticulitis is classified as a gastrointestinal disorder within the broader spectrum of digestive diseases. It occurs when small pouches, known as diverticula, form in the walls of the colon and become inflamed or infected. These diverticula develop due to increased pressure within the colon, often due to a low-fiber diet, constipation, and aging. As people age, the muscle layers of the colon can weaken, making it more susceptible to developing these pouches, which can range in size and number.
The colon's anatomy includes four main sections: the ascending colon, transverse colon, descending colon, and sigmoid colon, where diverticula are most frequently observed. If one or more of these diverticula become inflamed or infected, the condition known as diverticulitis arises. The inflammation occurs when waste material gets trapped in the diverticula, leading to irritation. In some cases, bacterial overgrowth within the pouches can lead to an infection, further aggravating the inflammation.
Patients suffering from diverticulitis may experience a variety of symptoms, including abdominal pain (commonly on the lower left side), fever, nausea, and changes in bowel habits. The severity of these symptoms can range from mild to severe. In some cases, complications such as abscess formation or colon perforation can occur, resulting in more serious health issues. Thus, early recognition and diagnosis of diverticulitis are essential for effectively managing and treating this gastrointestinal disorder.
Recognizing the Symptoms of Diverticulitis
Diverticulitis can manifest through a range of symptoms, primarily characterized by abdominal pain. Often, this pain is localized in the lower left quadrant of the abdomen, though it can occur on the right side, particularly in individuals of Asian descent. The nature of the pain varies; it can be moderate to severe and may start suddenly or develop gradually over time. Patients may experience sharp, cramping sensations that last from several hours to a few days, often exacerbated by movement or pressure.
In addition to abdominal pain, individuals with diverticulitis frequently report changes in bowel habits. These changes may present as constipation, diarrhea, or alternating episodes of both, which can further indicate the severity of the condition. Nausea and vomiting are common accompanying symptoms, often making patients feel unwell or unable to keep food down. Furthermore, a low-grade fever and chills may develop as the body fights inflammation, indicating an underlying infection.
It's important to note that symptoms can vary significantly from person to person, with some experiencing mild discomfort while others may have severe complications. If diverticulitis is left unmanaged, it could lead to significant complications such as abscess formation, perforation of the intestine, or peritonitis, which is a life-threatening condition. Early recognition of these symptoms is crucial for effective management and treatment, as addressing diverticulitis promptly can help prevent these potential complications.
Overall, being aware of the symptoms allows for timely medical intervention, improving the prognosis for those affected by this condition.
Diagnostic Procedures for Diverticulitis

The diagnosis of diverticulitis begins with a thorough medical history and physical examination. Patients typically report symptoms such as abdominal pain, fever, and changes in bowel habits, which guide healthcare providers in their assessment. The physical examination may reveal abdominal tenderness, specifically in the lower left quadrant, and palpation may elicit pain, suggesting inflammation.
Imaging tests play a crucial role in confirming a diagnosis of diverticulitis. Computed Tomography (CT) scans are the gold standard, providing detailed images that help differentiate diverticulitis from other conditions. Ultrasounds may also be employed, particularly in patients where radiation exposure should be minimized. These imaging studies visualise inflamed diverticula and can reveal complications such as abscesses or perforations.
Moreover, bowel examination procedures add another layer of diagnostic accuracy. Colonoscopy, for instance, allows direct visualization of the colon, helping to rule out other potential issues such as colon cancer or inflammatory bowel disease. While less common during acute settings due to the risk of perforation, it remains significant in chronic evaluations and follow-ups, ensuring a comprehensive understanding of a patient's gastrointestinal health.
Treatment Approaches for Diverticulitis
Diverticulitis can manifest in varying degrees of severity, directly influencing the treatment strategy employed. Mild cases typically involve inflammation without complications and may respond well to conservative management. In such instances, treatment options usually include dietary modifications, such as a shift to a low-fiber diet during flare-ups and over-the-counter medications to alleviate pain and reduce inflammation. Antibiotics may be prescribed to tackle potential infections resulting from diverticulitis, but their use is often reserved for more severe or recurrent symptoms.
In contrast, severe diverticulitis can present with complications such as abscesses, perforations, or significant blockages, necessitating more aggressive measures. Surgical intervention becomes necessary if these complications arise or a patient experiences recurrent episodes. The types of surgeries performed can range from less invasive approaches, such as laparoscopic surgery, which involves the removal of the affected segment of the colon, to more extensive procedures like colostomy, where a portion of the colon is diverted to an external pouch. Ultimately, the choice of treatment depends on the individual's overall health, the condition's severity, and any complications. For chronic cases, ongoing medical management and lifestyle changes may also be recommended to prevent future flare-ups, emphasizing the importance of a well-rounded approach to treatment.
Proactive Steps to Prevent Diverticulitis
To reduce the risk of diverticulitis, focus on a high-fiber diet rich in fruits, vegetables, whole grains, and legumes, which can help maintain healthy digestion. Incorporating regular physical activity into your routine not only aids digestion but also promotes overall wellness. Additionally, staying adequately hydrated is crucial; drinking plenty of water helps fiber do its job effectively. It's also essential to keep up with regular health check-ups and screenings to identify potential issues early on. Adopting these lifestyle changes can significantly lower your chances of developing diverticulitis and maintain good digestive health.





